Illustrations by Eva Giurco
Who is my Doctor?
Patients affected by DF are treated by surgeons and oncologists. DF is a tumor with a borderline behavior between benign and malignant, due to its characteristics of high local aggression, so the team must have the experience and skills necessary to care for patients with DF. Your treatment will be decided by a group of Doctors specialized in various branches of Medicine (multidisciplinary team) and usually you can find them in centers specialized in sarcoma’s treatment.
Which ones are they?
The optimal choice of medical and/or surgical therapy to offer the patient depends on various factors which may include:
- the localization and size of the tumor
- the presence of symptoms
- the rate of growth of the tumor
- its proximity to important organs such as blood vessels
- the patient’s preference, who plays a role in the choice once informed of the therapeutic options available, the toxicity profiles of the various drugs and their administration.
Each desmoid tumor has its own clinical behavior which can evolve differently over time: it can continue to grow, it can remain stable or even regress spontaneously. The behavior of DF is not predictable but if it regresses or remains stable it may not be treated.
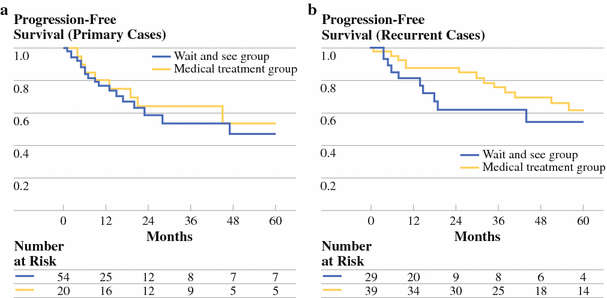
Therefore, considering the high number of recurrences, the morbidity related to surgery and the possibility of stability of the disease or even spontaneous regression also in absence of treatments, recently a more conservative treatment has been proposed and an initial surveillance approach has been suggested.
This ACTIVE SURVEILLANCE program, with clinical and radiological observation only, is defined as “Watch and Wait” protocol.
Active Surveillance
Active surveillance is typically the first approach for most people with a new diagnosis of DF. It’s defined as active monitoring or active observation (via FOLLOW UP). This monitoring program can be “slowed” after 1-2 years. A new patient that starts with active surveillance program may be concerned that his disease is not being treated immediately, but this approach has many advantages:
- Also if active treatments for DF are very effective, they have side effects however; therefore, it’s more rational to use them when the tumor is growing or it’s affecting the quality of life.
- Some of the treatments, such as radiotherapy, can only be repeated once. Radiotherapy is useful for reducing symptoms but it does not always stop the growth of DF and still it has side effects even in the long term (e.g. risk of radio-induced tumors)
- Surgical removal of DF may be related to high recurrence rates.
If the patient with desmoid fibromatosis is initiated into an active surveillance program, he will follow a regular monitoring program with his oncologist which includes checks every three to four months. At each appointment, the possibility of starting a treatment through a clinical examination and the study of radiological examinations (ultrasound or MRI) will be examined.
The reasons that lead the doctor to stop active surveillance and to start specific therapy are:
- a worsening of symptoms that may compromise quality of life (for example pain that cannot be managed with drugs)
- a rapid increase of tumor size
- a tumor growth that closes or compresses important structures such as organs, large blood vessels or nerves
- a continuous progression over time
Watch and wait
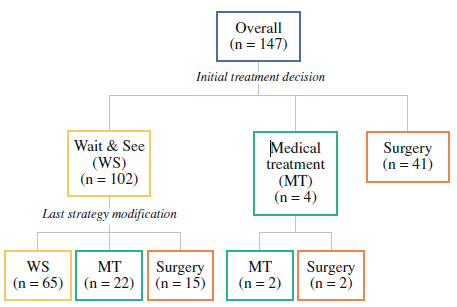
Algorithm
Treatments
THE TREATMENT WILL BE CHOSEN ACCORDING TO THE CHARACTERISTICS OF EACH PATIENT AND HIS DESMOID TUMOR. EACH CASE MUST BE DISCUSSED BY A MULTIDISCIPLINARY TEAM (MADE UP OF ONCOLOGISTS, SURGEONS, PATHOLOGISTS, RADIOLOGISTS AND PAIN THERAPISTS EXPERIENCED IN THE TREATMENT OF THE DESMOID FIBROMATOSIS) TO FIND THE BEST TREATMENT FOR EACH PATIENT.
If there is increase of tumor size or worsening of symptoms, medical treatment with drugs or other treatment options may be initiated, which are listed below.
Surgery
Until few years ago, surgery was considered the treatment of choice for patients with desmoid tumor and it involved the removal of the tumor with a large margin, that is associated with the removal of a large area of healthy tissue too. Despite the adequacy of the margins, the risk of disease recurrence has always been high and up to 70% described in the literature. Therefore, surgery does not guarantee that the tumor will not recur in the same localization.
This high risk, the need for multiple surgeries in patients with recurrences that is related with functional and aesthetic outcomes as well as the observation of stability in absence of treatment and some spontaneous regressions, led to a change in the therapeutic approach, thus avoiding surgery as an initial treatment.
This change in the clinical approach has not been correlated with a study regarding the pathogenetic mechanisms of progression. In the literature, in fact, only and exclusively data are available regarding the risk of disease recurrence related to some types of beta-catenin mutation, in patients treated with surgery.
The correlation between the type of mutation of the tumor and any spontaneous progression or regression in patients under control or the response to treatments has not been studied yet. Clinical-translational studies are underway to clarify some of these aspects.
To date, therefore, there are no prognostic factors that allow us to predict which treatment is the best for each patient. Today, surgery can still represent one of the therapeutic options and is shared with patients who have desmoids that show progression in favorable locations such as the abdominal wall. However, it is not proposed if important functional and aesthetic deficits are expected.
NSAID
Non-steroidal anti-inflammatory drugs (NSAID) can be used to treat DF. These drugs can have an impact on tumor growth and are also useful for treating the inflammation and pain associated with the tumor.
Their molecular target is the cyclooxygenase (COX-2). This is an enzyme that regulates prostaglandin synthesis and it plays an important role in many biological processes such as the regulation of immune function. The overexpression of COX-2 causes an increase in the expression of platelet-derived growth factors (PDGF) and this process can contribute to tumorogenesis, stimulating angiogenesis and invasiveness. Furthermore, COX-2 has also been associated with the promotion of resistance to apoptosis, for example by altering the relative levels of survivin and pro and anti-apoptotic proteins of the Bcl-2 family. The expression of COX-2 is elevated in several tumors, including desmoid tumor.
Celecoxib (Celebrex) is a NSAID used for the therapy of desmoid tumor, it would interfere with the regulation of anti-apoptotic proteins by inhibiting COX-2.
Another NSAID used for the treatment of DF is Sulindac: it works by inhibiting the synthesis of prostaglandins with its action on the COX enzyme.
Hormone therapy
Hormones are molecules naturally produced in the body that control the biological activity of cells. Hormone therapy uses drugs that interfere with the way of production or action of hormones.
Desmoid tumors are often sensitive to hormone therapy, particularly hormone therapy with anti-estrogenic activity. The anti-estrogen drugs Tamoxifen and Toremifene used in breast cancer are part of this therapy.
Both Tamoxifen and Toremifene have been shown to be active in DF. They are usually given in high doses, alone or in combination with NSAID. It’s still not clear which dosage is the best to use. They are generally used as first-line drugs in DF, especially if the tumor is localized on the abdominal wall.
The likelihood of achieving disease size reduction or clinical benefit with these drugs is actually quite low. However, it’s a therapy with an excellent tolerability profile and with the advantage of being oral administrating. Therefore, anti-hormonal therapy associated or not with anti-inflammatory therapy currently represents an option that can be proposed to patients with a favorable clinical situation in terms of localization and evolution, with a gradual approach to the disease.
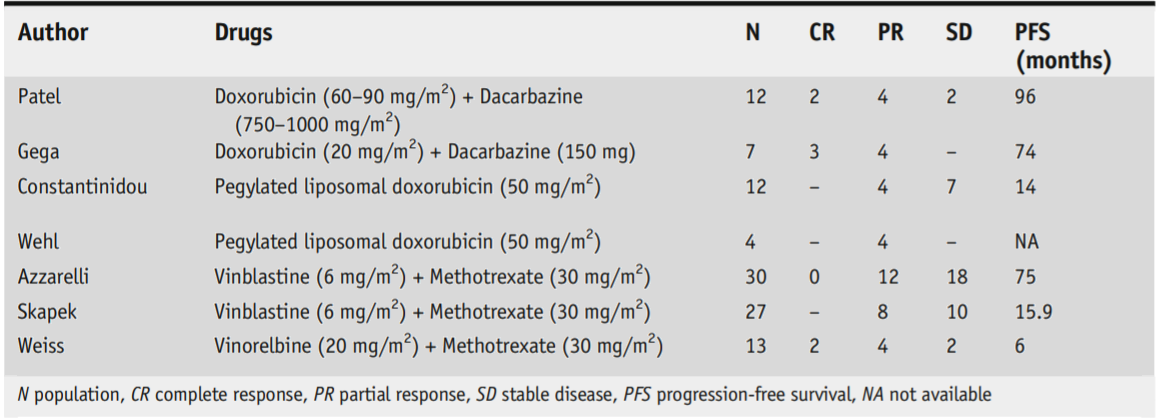
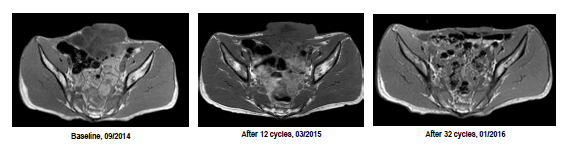
Chemotherapy
Chemotherapy is a treatment that involves the use of drugs to destroy cancer cells. Chemotherapy can also “turn off” the tumor by making the neoplastic cells “dormant”. These effects can help with symptoms caused by DF, such as pain. During chemotherapy the tumor may decrease in size or it may stop growing. Chemotherapy can cause various side effects so its use must be well thought out, considering the symptoms and the tumor speed of growth. This treatment is more likely to be chosen if the tumor is growing rapidly and there are symptoms that are not otherwise manageable. It should be considered after the failure of other therapeutic regimens such as those based on NSAID.
The most frequently used chemotherapy drugs are Methotrexate in combination with Vinorelbine/Vinblastine, with low dosage, for long periods. It is also possible to use another class of chemotherapeutic agents known as Anthracyclines, however these present a more toxic profile than traditional low-dose chemotherapy and therefore today this type of approach is offered only to a limited number of patients in particular clinic situations.
Low-dose chemotherapy is based on the use of drugs that are administered intravenously every week, for a long period of time (around a year). The toxicity profile of these drugs is quite good. In particular, severe side effects are very rare. More often there are mild or modest side effects concerning laboratory alterations, asthenia and nausea.
The weekly frequency of this therapy and the need to extend it over time can have an impact on the quality of life of patients. This aspect must certainly be considered and shared with the patient when starting therapy. On the other side, it’s an approach that has a high probability of obtaining a clinical benefit and a dimensional reduction of the disease, even if the radiological responses can be observed some time after the start of the treatment. Responses are generally maintained over a long time after the end of the chemotherapy treatment.
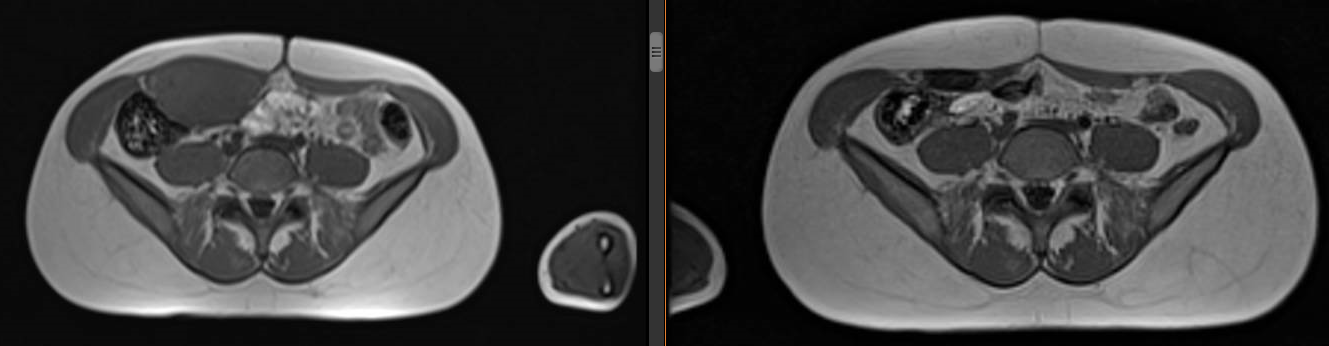
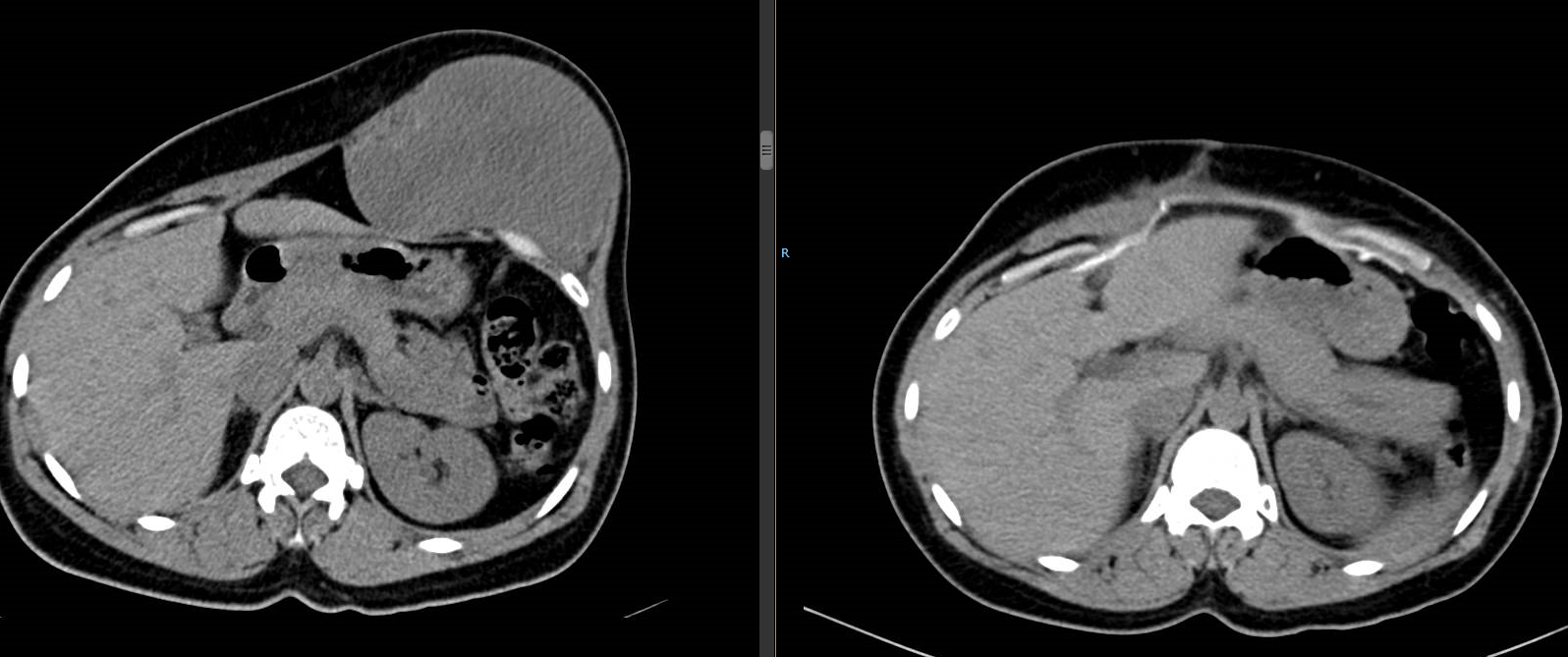
Mass regression
The tyrosine kinase inhibitors
This category of drugs targets tyrosine kinases which are cell membrane proteins that can be aberrantly activated in some tumors leading to pathological processes. In this sense, the use of tyrosine kinase inhibitors has an antitumor effect and is widely used in oncology.
In DF several drugs with anti-tyrosine kinase activity have been shown to be active:
- IMATINIB was the first drug of this category to have demonstrated efficacy in patients affected by DF.
- Furthermore, two clinical studies have been conducted on desmoid tumors in recent years with two different drugs belonging to this category: PAZOPANIB and SORAFENIB
The results of these two clinical studies were presented in June 2018 at the annual congress of the American Society of Medical Oncology and were positive for the percentage of dimensional responses obtained and also for the disease control maintained over time. In fact, 80% of patients treated with Sorafenib, two years after the end of treatment, had not shown a progression of the disease. The oral administration of these drugs is an advantage but on the other side toxicity is not absent and can sometimes be difficult to manage.
It’s important to underline that in Italy Sorafenib is not available today for patients with desmoid tumor while Pazopanib can be used in patients with this disease, in addition to the medical options already available.
FUTURE PERSPECTIVES
Several clinical trials are currently underway on new drugs that could have a potential effect on desmoid tumor, but we still await the long-term results. Among these are:
- NIROGACESTAT: Among the new drugs with promising activity in desmoid tumors, nirogacestat, which targets the Notch pathway, must certainly be mentioned.
This pathway is involved in the regulation of many physiological processes but it can also be involved in some pathological processes including tumor development. In this sense, the inhibition of this pathway can have an antitumor effect.
Nirogacestat was tested in a very early clinical study, demonstrating a very good tolerability profile and a truly peculiar activity in desmoid tumors albeit on a very small number of patients. These preliminary data were then confirmed in a subsequent phase II study, again on a limited number of patients.
Currently, with the aim of confirming these preliminary data on a larger population of patients, a phase III study is underway with this drug, on an international level, with a population of patients with desmoid tumor that has shown a progression before entering the trial. This study is already active in the United States, where it’s enrolling patients, and it will soon be approved and opened in Europe and Italy.
** For more information on the clinical study about Nirogacestat, download the brochure **
- TEGAVIVINT: Among the various future options for the treatment of desmoid tumors is that of using drugs that directly target the β-Catenin pathway, which is unregulated both in sporadic desmoid tumors and in patients with FAP, causing an accumulation of β-Catenin inside the nucleus which leads to the transcription of genes involved in cell proliferation. This is why TEGAVIVINT was developed, a drug that targets beta-catenin, which has been shown to have a cytotoxic action in some preclinical models of desmoid tumor. The Phase I study of this drug was launched in the USA.
Radiotherapy
Radiotherapy uses high-energy beams of radiation to destroy cancer cells. This treatment can be used after surgery or on its own; it is intended to improve symptoms and to attempt to slow tumor growth. Its use is influenced by the tumor anatomical localization.
Patients with DF are generally young and radiotherapy can have side effects that also occur in the long term, therefore his use must be well considered and it’s usually not the first choice for children and young adults. It is more indicated in older patients, when the drug treatment is not active or cannot be administered due to comorbidity or low tolerance.
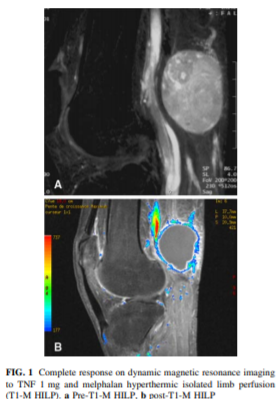
Hyperthermic-antiblastic isolated perfusion of the limb
Perfusion (ILP) is a therapeutic option for patients with desmoid tumors of the distal extremities (forearm/hand or leg/foot). It involves complete vascular isolation and the perfusion of the limb is performed in extracorporeal circulation with oxygenated and heated blood through a circuit in which chemotherapy drugs (Melphalan) and cytokines (TNF) are inserted. Not all centers have the opportunity to perform this treatment; if a patient needs this treatment, he can be referred to specialized centers.
Cryoablation
Cryoablation can be used to treat DF; it’s based on the use of very low temperatures to freeze the tumor. A needle called cryodispenser is inserted into the tumor then a gas is injected to freeze the tumor. This technique can be used for small and localized tumors close to the skin. This technique is not available in all centers; if a patient needs this treatment, he can be referred to specialized centers.
HIFU
It’s a new technique used mostly in US and Australia, for which there is not yet enough long-term data and it’s practiced only in a few highly specialized centers. It uses high-intensity ultrasound, it represents a non-invasive method that heats and destroys pathogenic tissues. However, this treatment requires a patients selection based on the proximity of the tumor to nervous or superficial structures and/or the presence of previous scars.
TREATMENT of Desmoid Tumor
OBSERVATION represents the first therapeutic approach to this disease. When the disease maintains its evolutionary trend, it requires the initiation of a specific treatment.
This specific treatment depends on the anatomical localization of the disease, the speed of growth and the choice of the patient.
There are four specific localizations that require approaches which can be different:
ABDOMINAL WALL
In this localization there is the highest percentage of spontaneous regressions. When desmoid fibromatosis in this site does not stop its growth it’s required a treatment, which often in the first instance, and ONLY IN THIS LOCALIZATION, can be a surgery, because they are easily treated surgically. The surgery here is favorable and hasn’t many side effects on the quality of life. It’s a decisive surgery in the majority of cases, in fact it’s estimated that in 95% of cases it’s not followed by any recurrence.
If the surgery is not effective or the patient does not want to do it, in general, the treatment that is proposed for the progressing abdominal wall fibromatosis is hormonal treatment. If this treatment is not effective, we move on to a low-dose chemotherapy treatment or to a latest generation molecular therapy.
INTRADOMINAL LOCALIZATION
We refer to mesenteric fibromatosis, which are rare in the sporadic form and are frequent in association with FAP. In these cases, once the initial observation has failed, the primary treatment is low-dose chemotherapy. Today, as an alternative to low-dose chemotherapy, we can certainly consider the use of the latest generation of molecular therapies. If these treatments are not possible or are not effective, a more aggressive chemotherapy treatment is generally proposed because in this localization the tumor progression can determine the involvement of important anatomical structures with significant impairment of the quality of life and in some cases with possible fatal outcomes. Surgery is generally considered after a size reduction to carry out an overall conservative surgery and only in extremely selected cases. Generally this does not happen in the familial forms, that is associated with polyposis, but it can occasionally happen in the sporadic forms. Furthermore, in patients with FAP, the risk of new desmoids following surgery must be considered.
LIMBS AND TRUNK – THORACIC WALL
Limbs and girdles are important and complicated sites as functional point of view since they can determine the involvement of muscular and even nervous structures, causing important consequences and deficits. These localizations most easily affect young people and pediatric patients and these are the most difficult to treat surgically since here the surgery is very often followed by a local recurrence and involves functional sacrifices of the limb/area. So surgery in these cases represents a last treatment, where all available therapies fail. The choice of treatment depends on the speed of growth. DF that grow slowly are addressed in the first instance with hormonal treatments, DF that grow faster are treated with low-dose or conventional chemotherapy and with molecular drugs.
HEAD/NECK
It represents one of the rarest and most critical localization because when DF develops in the structures of the neck, mainly, given the continuity with vital structures such as the airways (for example the trachea or larynx) and the digestive tracts (such as the esophagus), make the treatment of these tumors more complicated and delicate. Large tumor growths cannot be observed without treatment because the neck space is very limited. So, often in this localization a more contained observation is required, more limited in time, and more quickly it becomes necessary to establish a treatment which, in these cases, is often chemotherapy and possibly molecular rather than surgical. Also in these cases the surgery is considered as last therapy. More easily, if the medical treatment does not work, a loco-regional radiotherapy treatment is considered for these sites. These localizations are easily observed in later life, sometimes associated with/subsequent to surgical treatments of the head and neck.
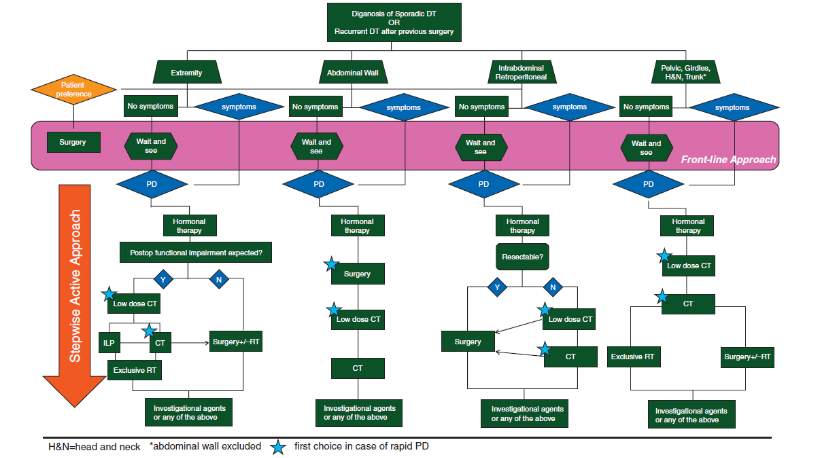
Algorithm
Active surveillance without any treatment
After active surveillance: progression of the tumor, surgical treatment
WARNING! Informations on this site are designed to improve and to inform the patient and in general to promote greater awareness of their pathology. In no case they replace specialist medical advice. While guaranteeing the accuracy and scientific rigor of the information, DESMOID FOUNDATION declines all responsibility about informations provided on the treatments, reminding all patients to contact their specialist doctor and to evaluate with him the best treatment in a specific personal case.
